Angels Den 2025
From a small classroom at St. Michael’s Hospital to a live show at Koerner Hall, Angels Den has grown to become Canada’s biggest medical research competition.
On Wednesday, October 22, 2025, St. Michael’s all-star scientists will once again pitch their life-changing ideas for a chance at winning critical research funding.
It's time to usher in a new era of medical discovery.
Enter for a chance to win tickets here or to learn more, contact Amy Lewis.
The Awards
Keenan Award for Medical Discovery
Transforming scientific discoveries into novel therapies, better diagnostics, vaccines or medical devices.
Mitchell Award for Health System Innovation
Improving our healthcare system by increasing its effectiveness, efficiency, equitability or sustainability.
Canada Life People’s Choice Award
Favourite research project in any category, voted for by the audience.
Sarah McComb Award for Cancer Research
Spurring research to improve the diagnosis and treatment of cancer.
Meet the Teams
Keenan Award for Medical Discovery
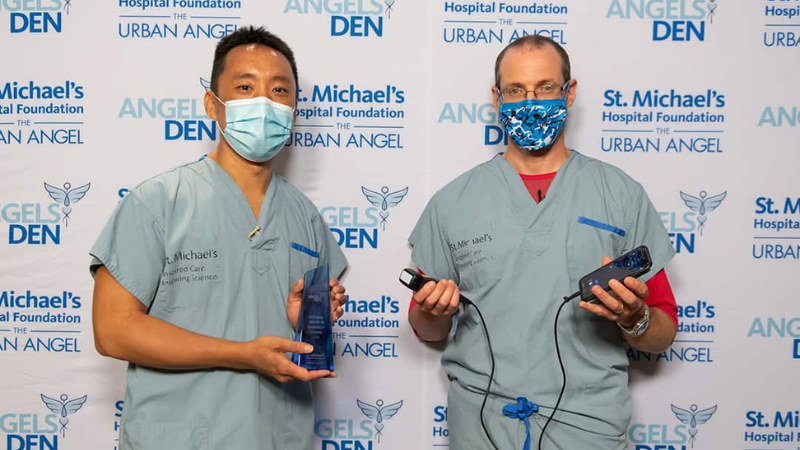
Instant Insight: Bedside Imaging for Lung Injury
Eno Hysi, PhD | Dr. Warren Lee
Eno Hysi, PhD
Physicist and Scientist, Keenan Research Centre for Biomedical Science, and The Nicole and Thor Eaton-Canada Research Chair in Quantitative Ultrasound and Photoacoustic Imaging, St. Michael’s Hospital
Dr. Warren Lee
Critical Care Physician, Clinician-Scientist, Keenan Research Center for Biomedical Science, and Canada Research Chair in Mechanism of Endothelial Permeability, St. Michael’s Hospital
THE CHALLENGE: Acute respiratory distress syndrome (ARDS) is a serious lung condition that can develop following respiratory infections or trauma. Diagnosing and monitoring currently relies on X-rays and CT scans, which can be slow, imprecise, and carry risks related to patient transport and radiation exposure.
THE SOLUTION: Dr. Warren Lee and Eno Hysi have developed a bedside ultrasound device that makes diagnosing and monitoring ARDS faster, easier, and safer. This radiation-free technology uses light and sound to image lung oxygen levels in real-time, helping doctors respond more quickly and accurately.
Keenan Award for Medical Discovery
Pregnancy Protector: Targeted Care for Two
Dr. Hagar Labouta | Luis Pérez Dávalos MD
Dr. Hagar Labouta
Scientist, Keenan Research Centre for Biomedical Science, and Keenan Professor in Medical Discovery, St. Michael’s Hospital
Luis Pérez Dávalos, MD
PhD Student, Keenan Research Centre for Biomedical Science, St. Michael’s Hospital
THE CHALLENGE: Three out of four pregnant women take medication—yet for 70% of those drugs, we don’t know if they’re safe for the baby. Even more concerning: 1 in 10 are known to cause harm, but doctors have no safer options to offer.
THE SOLUTION: Drs. Labouta and Pérez Dávalos are developing a breakthrough drug delivery system that targets treatment to the mother only, shielding the baby from potential unknown side effects. This innovation could transform care for a wide range of conditions—from cancer to epilepsy and more.
Keenan Award for Medical Discovery
Precision Psychedelics: Getting Treatment Right the First Time
Dr. Katharine Dunlop | Dr. Akash Goel
Dr. Katie Dunlop
Scientist, Keenan Research Centre for Biomedical Science and the Centre for Depression and Suicide Studies, St. Michael’s Hospital
Dr. Akash Goel
Anesthesiologist and Clinician-Investigator, Li Ka Shing Knowledge Institute, St. Michael’s Hospital
THE CHALLENGE: Chronic neuropathic pain affects more than one in 10 Canadians, with many describing their experience as “worse than death.” More than half also struggle with major depressive disorder, making treatment more complex and often necessitating a long cycle of trial and error to find the correct therapy.
THE SOLUTION: Drs. Katharine Dunlop and Akash Goel are developing a first-of-its-kind AI tool that classifies patients with chronic pain and depression based on the unique pattern of their brain activity, which acts like a neural fingerprint. These patterns can be used to predict which psychedelics (ketamine, MDMA, psilocybin) will help each patient, offering more personalized care for those with chronic pain and depression.
Award for Health System Innovation
Elite Fleet: Trauma Team to the Scene
Dr. Sheldon Cheskes | Dr. Johannes von Vopelius-Feldt
Dr. Sheldon Cheskes
Emergency and EMS Physician, Clinician-Scientist, Li Ka Shing Knowledge Institute, St. Michael’s Hospital
Dr. Johannes von Vopelius-Feldt
Emergency Physician, Clinician-Scientist, Li Ka Shing Knowledge Institute, St. Michael’s Hospital
THE CHALLENGE: Trauma is the leading cause of death for Canadians under 40, with 60% of major trauma patients dying before ever reaching a hospital. Emergency doctors can save lives, but only once patients arrive in the ED. In the GTA, that trip takes an average of 43 minutes for severely injured patients—and every minute counts.
THE SOLUTION: Drs. Johannes von Vopelius-Feldt and Sheldon Cheskes are reimagining emergency medicine with Critical Care Response Units that bring the ER to the scene. These specialized physician-paramedic teams can be dispatched directly to critically injured patients, delivering faster trauma care, and saving lives.
Award for Health System Innovation
Dependable Dialysis: No Surgery Required
Dr. Monica Farcas | Dr. Jeffrey Perl
Dr. Monica Farcas
Urologist, Surgeon-Scientist, Li Ka Shing Knowledge Institute, and Agnico Eagle Mines Professorship in Minimally Invasive Urology and Endourology, St. Michael’s Hospital
Dr. Jeffrey Perl
Nephrologist and Clinician-Investigator, Li Ka Shing Knowledge Institute, St. Michael’s Hospital
THE CHALLENGE: Dialysis is a lifeline for people with kidney failure, removing waste and toxins from the body. Peritoneal dialysis involves filtering fluids through a catheter in the abdomen that gives patients the ability to receive treatment at home. However, if the catheter becomes blocked, the results can be devastating, requiring emergency surgery.
THE SOLUTION: Drs. Monica Farcas and Jeffrey Perl have invented the DialySnake, a device that quickly and effectively clears these catheters. No hospital stays. No costly surgery. No risky general anesthesia. It’s a safer, faster, and far more affordable alternative that could change the lives of dialysis patients.
Award for Health System Innovation
Goodbye Gridlock: Leveraging AI to End Hallway Medicine
Michael Page | Dr. Jennifer Watt
Michael Page
Director, AI Commercialization, St. Michael’s Hospital
Dr. Jennifer Watt
Geriatrician and Clinician-Scientist, Li Ka Shing Knowledge Institute, St. Michael’s Hospital
THE CHALLENGE: One in six hospital beds in Canada are occupied by patients who no longer need hospital care but are waiting for rehab, long-term care, or social supports. This backlog is partly caused by challenges in collecting key data in busy emergency departments, and doctors not always being able to recognize patients at risk of extended stays.
THE SOLUTION: Dr. Jennifer Watt and Michael Page are leading the development of an innovative AI-driven tool that identifies elderly patients at risk of prolonged hospital stays. This technology will empower care teams to intervene earlier, helping to shorten hospital stays and improve patient outcomes through safer, more coordinated discharge processes.
Meet the Host and Judges

Nick Dixon - Host
Nick Dixon is the co-anchor of CP24 Breakfast , Toronto’s #1 morning show—though fun fact, he’s not even a morning person. For more than 25 years, he’s been covering top stories and breaking news in the GTA and beyond, as well as reporting on some of the biggest events in Canada and around the world. Off-air, he’s busy chasing his three energetic kids and practicing his pickleball swing for Paddle Royale.
Amanda Lang - Judge

Bruce Croxon - Judge
Bruce Croxon made his mark as a digital trailblazer by co-founding Lavalife. Since selling the company, he’s stayed close to the action—investing in and advising a number of growing tech companies. Bruce spent three seasons on CBC’s hit show Dragons’ Den, and later co-founded Round13, an investment fund that helps Canadian tech businesses scale. He’s also a regular voice on BNN and, most recently, launched a charitable initiative called 13thround.life, using the sport of boxing to empower at-risk youth.

Samantha Yammine - Judge
Dr. Samantha Yammine, PhD is a Neuroscientist turned Science Communicator better known as Science Sam. As @science.sam on Instagram and TikTok, she’s an innovative leader in making science more familiar, accessible, and inclusive. She is the host of Curiosity Weekly, the flagship science podcast for Discovery, and a Regular Science Expert on CTV’s daily lifestyle show The Good Stuff with Mary Berg. Samantha is the Chair and a Co-Founder of the award-winning non-profit Science is a Drag, and sits on the Advisory Board for the anti-misinformation organization ScienceUpFirst.
Thank You To Our Sponsors
Presenting Sponsor
.png)
Top Prize Sponsor
People’s Choice Award Sponsor

Team Biographies Sponsor
.png)
Team Award Sponsors





NextGen Sponsor

Corporate Jurors













Jurors
Frank Balazic, PBY Capital
Greg & Susie Belton
Keri Bush
Tony Cesta
David Cooper
Mark Curry
Scott K. Fenton, Fenton Law Barristers
The Fowler Family
Savita Gupta
Margaret Harvey
Elaine Kierans & Shawn
McReynolds
The Krembil Foundation
Barbara Lemaire
Robert Macdonald, Bond Brand Loyalty
Mariana MacIntosh
Joe Mazzocco
Mary Mullen
Brian O’Connor
Harcharan (Harry) Singh
Dan & Sandra Sullivan
Kristine Thompson
Special Thanks To
Epic
Tim and Darka Griffin
Colleen Johnston
Leon's
Pat Meneley
Raymond James
The Toronto Star
St. Michael’s Hospital Department of Emergency Medicine
St. Michael’s Hospital Department of Medicine
St. Michael’s Hospital Department of Psychiatry
St. Michael’s Hospital Department of Surgery
Our Committee
Melissa Martin, Co-Chair
Gillian Riley, Co-Chair
Ram Amarnath
Keri Bush
Max Celej
Dr. Erica Conte
Mariana MacIntosh
Jeff Marshall
Wes McComb
Amit Monga
Mike Quinn
Bill Pringle
Tony Rodrigues
Dr. Ori Rotstein
Nicole Svec
Kate Yurincich
Join the Research Innovation Council
Want to go behind the scenes of medical research and launch a life-changing project? You can.
The Research Innovation Council is an exclusive group that chooses top scientists to receive RIC funding to launch their research projects. This is your chance to impact some of the toughest and timeliest health issues – like those you’re watching on Angels Den. Invest $10,000 per year over five years – and make medical ingenuity possible.
Contact Chanel to join.
Media
.png)
Angels Den is Canada’s largest medical research competition
It's Canada's largest medical research competition, giving doctors and scientists an added jolt to get their work off the ground.
Watch.png)
Toronto scientists develop new scan to improve kidney diagnostics
Scientists at St. Michael's Hospital in Toronto have developed technology that can scan and more accurately diagnose kidney problems.
Watch.png)
AI model developed at Toronto hospital helps doctors triage brain surgery
A team of St. Michael's doctors has developed an innovative AI model designed to assist in the complex decision-making process regarding brain surgery for patients.
Watch.png)
Scientists vie for pitch competition prize money in Toronto
A pitch competition is helping researchers get their work off the ground, with the hopes of seeing new therapies and technologies developed to help patients.
WatchPast Winners
Canada Life People's Choice Award, $100,000
Surviving Sepsis: A Breakthrough Drug
Dr. Claudia dos Santos and Dr. Amin Ektesabi
THE CHALLENGE: Sepsis is a life-threatening medical emergency caused when the body’s response to an infection injures its own tissues and organs. Worldwide, there are 50 million cases each year. As the only treatments are antibiotics, which aren’t always effective, and organ support, one in five people will die from this common hospital complication.
THE SOLUTION: Dr. Claudia dos Santos and Dr. Amin Ektesabi have developed a breakthrough drug to block inflammation, supercharge the white blood cells’ ability to kill bacteria, and protect against heart and lung failure. Now they want to test it in pre-clinical trials–so they can move quickly to save lives.
Keenan Award for Medical Discovery, $250,000
No More Needles: A Non-Invasive Way to See Kidney Scarring
Dr. Darren Yuen
THE CHALLENGE: Chronic kidney disease – caused when diabetes or high blood pressure irreversibly damages the organs by scarring them – affects one in 10 Canadians. The usual way to diagnose kidney disease is by a needle biopsy. Not only is the procedure painful, it can be dangerous: it may cause bleeding, sending patients to the ICU.
THE SOLUTION: Dr. Darren Yuen has developed a simple, non-invasive ultrasound scan that can take a picture of the kidney to see if there is scarring and how extensive it is. This first-of-its-kind innovation will revolutionize care for people around the world who are living with chronic kidney disease.
Odette Award for Health Systems Innovation, $250,000
AI Surgical Consult: Is Brain Surgery Needed?
Dr. Christopher Witiw and Dr. Alun Ackery
THE CHALLENGE: 165,000 Canadians will suffer a traumatic brain injury (TBI) this year. TBIs can cause serious long-term disability and even death. In fact, it’s the leading cause of death in young people. A rapid diagnosis and transfer to a hospital with a neurosurgeon are critical to save lives. But only one in five cases will end up needing surgery – and as it is, neurosurgeons are overwhelmed by the volume of consults.
THE SOLUTION: Dr. Christopher Witiw and Dr. Alun Ackery have developed an AI-based tool trained using brain imaging from thousands of TBI patients to help doctors decide who will need to undergo surgery. Now they want to test it at community hospitals without a neurosurgeon on staff to see if they can improve system-wide efficiencies.
Sarah McComb Award for Cancer Research, $150,000
Brain Waves: A New Treatment to Target Tumours
Dr. Vitor Periera
THE CHALLENGE: Meningiomas are the most common type of primary brain tumour in adults. They begin in the brain and spinal cord. The standard protocol is surgery to remove as much of the tumour as possible, followed by radiation therapy. However, open brain surgery is an extremely high-risk procedure and standard radiation therapy is not precise leading to side effects of exposing health brain tissue. We need new non-invasive ways to provide targeted treatment for brain tumours.
THE SOLUTION: Dr. Vitor Pereira has designed a procedure that delivers a radioactive particle directly to the site of the tumour through a series of tiny catheters. The catheters enter the body through the wrist or groin, instead of through the skull. This procedure has shown promise for liver cancer. Now, they want to determine if it is safe and effective for brain cancer.









.png)
.png)